Immune Regulation
TEL +81-6-6879-4957
FAX +81-6-6879-4958
Overview
Introduction to our Laboratory.
The discovery of interleukin 6 (IL-6) and elucidation of its associated receptor signaling pathway, highlighted the important role of cytokines in regulating immune cells. When cytokines become aberrantly regulated, this leads to the inappropriate activation of immune cells. In some cases, this is an important step in the development of autoimmune diseases, such as rheumatoid arthritis (activation of IL-6 signaling) and systemic lupus erythematosus (activation of type-I interferon signaling). The current challenges, and principal aims of our research, are to make advances in our understanding of the mechanisms of autoimmune disease and related cytokine signaling pathways, to ultimately improve health care- thus "from bench to bedside".
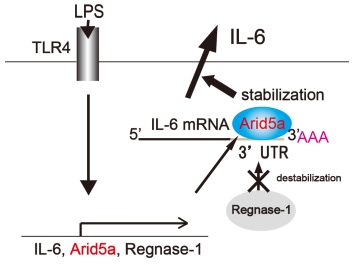
A Summary of our Recent Research. Arid5a controls IL-6 mRNA stability, which contributes to elevation of IL-6 level in vivo
Post-transcriptional regulation of IL-6 has been largely uncharacterized, with the exception of the RNase Regnase-1, which prevents autoimmunity by destabilizing IL-6 mRNA. Here, we identified a novel RNA binding protein, AT-rich interactive domain 5a (Arid5a), which stabilizes IL-6 but not TNF-α mRNA through binding to the 3' untranslated region (UTR) of IL-6 mRNA. Arid5a was enhanced in macrophages in response to LPS, IL-1β and IL-6. Arid5a deficiency inhibited elevation of IL-6 serum level in LPS-treated mice, and suppressed IL-6 levels and the development of TH17 cells in experimental autoimmune encephalomyelitis (EAE). Importantly, Arid5a inhibited the destabilizing effect of Regnase-1 on IL-6 mRNA. These results indicate that Arid5a plays an important role in promotion of inflammatory processes and autoimmune diseases.
Aryl hydrocarbon receptor-mediated induction of miR-132/212 cluster enhances TH17 cell differentiation
Aryl hydrocarbon receptor (AHR) has critical roles in autoimmune diseases such as multiple sclerosis (MS) by controlling Interleukin 17 (IL-17)-producing T helper cells (TH17 cells) and Regulatory T cells (Treg cells). Although various transcription factors and cytokines have been identified as key participants in TH17 generation, the role of microRNA is poorly understood. We found that miR-132/212 cluster is induced by AHR activation under TH17 -inducing, but not Treg cell-inducing conditions. miR-132/212 cluster deficiency abrogated enhancement of TH17 cell differentiation by AHR activation. We identified Bcl-6, a negative regulator of TH17 cell differentiation, as a potential target of miR-132/212 cluster. We investigated the roles of miR-132/212 cluster in experimental autoimmune encephalomyelitis (EAE), a murine model of MS. miR-132/212 cluster deficient mice showed resistance to the development of EAE and decreased frequency of both TH1 and TH17 cells in draining lymph nodes. Our findings indicate the novel mechanism of AHR-dependent TH17 cell differentiation via miR-132/212 cluster.
Type-I interferon controls its own production in immune homeostasis by inducing PPAR-γ expression and an inhibitory PPAR-γ/IRF7 complex
Type-I interferon is important for anti-viral immunity, but its over-production is linked to the development of autoimmunity. Type-I interferon production requires the transcription factor IRF7. How type-I interferon signals to attenuate its own production in immune homeostasis is not known. Here we show that type-I interferon induces expression of PPAR-γ, which forms an inhibitory interaction with IRF7, attenuating type-I interferon production via the virus-activated (MyD88-independent) pathways in fibroblasts and TLR-activated (MyD88-dependent) pathways in pDCs, and type-I IFN-dependent responses in autoimmunity. Thus all aspects of the type-I IFN system, its production in innate and adaptive immunity and associated immunopathology, are self-controlled through a two-step process of (i) type-I IFN-induced PPAR-γ expression and (ii) formation of an inhibitory PPAR-γ/IRF7 complex.
Therapeutic targeting of the interleukin-6 receptor.
Our research is engaged in clinical studies on the effectiveness of anti-IL6R antibody (Tocilizumab) in autoimmune diseases.
Tocilizumab can inhibit bone resorption and joint destruction in chronic rheumatoid arthritis (RA) patients by a large-scale randomized control trial. This effect is due to the inhibitory effect of IL-6 signal blockade on the expression of Rank-ligand and differentiation into osteoclasts of mononuclear cells.
A randomized placebo-controlled phase III trial confirmed that Tocilizumab is effective and safe in patients with systemic-onset juvenile idiopathic arthritis (JIA). The USA and EU approved the use of Tocilizumab for the treatment of JIA. In December 2012, large-scale clinical trials for JIA in Europe and the USA confirmed efficacy and safety of Tocilizumab.
Other autoimmune inflammatory diseases have been treated with Tocilizumab, including refractory relapsing polychondritis, AA amyloidosis, reactive arthritis, polymyalgia rheumatica, systemic sclerosis, polymyositis and acquired hemophilia A. The results confirmed efficacy and safety of Tocilizumab in these diseases.
Principal Investigator
Tadamitsu Kishimoto Professor

Research field
Mechanism of Treg/Th17 cell differentiation by IL-6 Anti-IL6 receptor antibody for the treatment of inflammatory diseases
Education history
| 1969.3 | graduated Osaka University Medical School |
|---|
Research and career history
| 1974.11 | Assistant Professor, Osaka University Medical School (1974.11) |
|---|---|
| 1979.4 | Professor, Osaka University Medical School |
| 1983.7 | Professor, Institute for Molecular and Cellular Biology, Osaka University |
| 1995.8 | Dean, Osaka University Medical School |
| 1997.8 | President, Osaka University |
| 2003.9 | Professor, Graduate School of Frontier Biosciences, Osaka University |
| 2011.9~ | Professor, Osaka University Immunology Frontier Research Center |
Prize
| 1988 | Asahi Prize |
|---|---|
| 1991.4 | Foreign Associate, The US National Academy of Science |
| 1992.6 | Imperial Prize from the Japan Academy |
| 1995.12 | Member, the Japan Academy |
| 1998.11 | The Order of Culture from Emperor |
| 2003.10 | Robert Koch Gold Medal |
| 2009.5 | The Crafoord Prize |
| 2011.1 | Japan Prize |
| 2017.1 | King Faisal International Prize |
| 2019.9 | The Keio Medical Science Prize |
| 2020.6 | Tang Prize |
| 2021.9 | Clarivate Citation Laureate 2021 |
Kang Sujin Associate Professor

Research field
Interaction of blood vessels with tissue-resident immune cells
Education history
| 2005.09 | M.S. Graduate school of engineering, Osaka University |
|---|---|
| 2012.03 | Ph.D. Graduate school of medicine, Osaka University |
Research and career history
| 2011-2012 | Young Scientist Research Fellow, JAPAN Society for the Promotion of Science |
|---|---|
| 2012-2014 | Assistant Professor, Institute for Academic Initiatives, Osaka University |
| 2014-2017 | Assistant Professor, Dept. of clinical application of biology, Graduate school of medicine, Osaka University |
| 2017-2021 | Assistant Professor, Lab. of Immune Regulation, iFReC, Osaka University |
| 2021-present | Associate Professor, Lab. of Immune Regulation, iFReC, Osaka University |
Prize
| 2020 | Osaka University Prize |
|---|---|
| 2020 | Young Scientists’ Award, The Commendation for Science and Technology by MEXT |
| 2018 | JSI Young Investigator Award, Japan Society of Immunology |
Members
-
Tadamitsu Kishimoto Professor
kishimotoifrec.osaka-u.ac.jp -
Kang Sujin Associate Professor
kangifrec.osaka-u.ac.jp
Publications (Tadamitsu Kishimoto)
- IL-6 and its receptor ; A paradigm for cytokines. Science 258: 593-597 1992.
- Cytokine signal transduction. Cell 76: 253-262 1994.
- Structure and function of a new STAT-induced STAT inhibitor-1. Nature 387: 924-929 1997.
- Interleukin 6: from bench to bedside. Nat Clin Pract Rheumatol. 2(11): 619-626 2006.
- IL-6-dependent and -independent pathways in the development of interleukin 17-producing T helper cells. Proc. Natl. Acsd. Sci. USA. 104: 12099-12104 2007.
- Efficacy and safety of tocilizumab in patients with systemic-onset juvenile idiopathic arthritis: a randomised, double-blind, placebo-controlled, withdrawal phase III trial. Lancet. 371(9617): 998-1006 2008.
Publications (Kang Sujin)
- Kishimoto T* and Kang S*. IL-6 Revisited: From Rheumatoid Arthritis to CAR T cell Therapy and COVID-19. Annu. Rev. Immunol. 40:323-48, 2022 (*Equally contributed)
- Kang S*, Kishimoto T*. Interplay between interleukin-6 signaling and the vascular endothelium in cytokine storms. Exp Mol Med. 12:1-8. 2021 (*Corresponding author)
- Kang S, Tanaka T, Inoue H, Ono C, Hashimoto S, Kioi Y, Matsumoto H, Matsuura H, Matsubara T, Shimizu K, Ogura H, Matsuura Y, Kishimoto T. IL-6 trans-signaling induces plasminogen activator inhibitor-1 from vascular endothelial cells in cytokine release syndrome. Proc Natl Acad Sci U S A., 117(36): 22351-22356, 2020
- Kang S, Narazaki M, Hozaifa M, Kishimoto T. Historical overview of the interleukin-6 family cytokine. J Exp Med. 217(5); e20190347, 2020
- Kang S*, Kumanogoh A*, The spectrum of macrophage activation by immunometabolism. Int Immunol. 16:dxaa017, 2020, (*Corresponding author)
- Kang S, Tanaka T, Narazaki M, Kishimoto T. Targeting Interleukin-6 Signaling in Clinic. Immunity, 50(4):1007-1023, 2019
- Kang S*, Nakanishi Y, Kioi Y, Okuzaki D, Kimura T, Takamatsu H, Koyama S, Nojima S, Nishide M, Hayama Y, Kinehara Y, Kato Y, Nakatani T, Shimogori T, Takagi J, Toyofuku T, Kumanogoh A*. Semaphorin 6D reverse signaling controls macrophage lipid metabolism and anti-inflammatory polarization. Nat Immunol. 19 (6), 561-570, 2018 (*Corresponding author)
- Kang S, Tanaka T, Kishimoto T. Therapeutic uses of anti-interleukin-6 receptor antibody. Int Immunol. 27(1):21-9. 2015
- Kang S, Kumanogoh A. Semaphorins in bone development, homeostasis, and disease. Semin Cell Dev Biol. 24(3):163-71. 2013
- Kang S, Okuno T, Takegahara N, Takamatsu H, Nojima S, Kimura T, Yoshida Y, Ito D, hmae S, You DJ, Toyofuku T, Jang MH, Kumanogoh A. Intestinal epithelial cell-derived semaphorin 7A negatively regulates development of colitis via αvβ1 integrin. J Immunol. 1;188(3):1108-16. 2012
